Neck pain is a major
public health care problem, with the prevalence of neck pain in the general
population ranging from 16.7% to 75.1% (mean 37.2%) and a lifetime prevalence
of 48.5% (1,2). Mechanical neck pain (MNP) was defined as
generalized neck pain and/or shoulder pain with mechanical features including
symptoms aggravated by maintained neck posture, movement or palpation of
cervical musculature (3). The etiology of MNP is not clear, however, it is
thought to be multifactorial.
Various cervical structures, such
as uncovertebral and intervertebral joints, neural tissues, discs, muscles or
ligaments may be the source of neck pain. It is also claimed that myofascial
trigger points localized in different head, neck, shoulder or upper back
muscles, and paracervical muscle spasm may be responsible for MNP (2).
Kinesiotaping
A
popular treatment technique used by physiotherapist in the management of
musculoskeletal pathologies is kinesiotaping (KT).
We want to know the effects of KT
in MNP, so we found a paper which study thirty-six patients (10 men, 26 women) with
regards to pain intensity, range of motion (ROM), disability, quality of life,
and depressive symptoms.
(Information extracted from: Onat
SS, Polat CS, Bicer S, Sahin Z, Tasoglu O. Effect of Dry Needling Injection and
Kinesiotaping on Pain and Quality of Life in Patients with Mechanical Neck
Pain. Pain Physician. 2019 Nov;22(6):583-589. PMID: 31775405)

KT Application
KT application is shown in Fig. 1.
The first layer of tape, a Y-strip, was placed over the posterior cervical
extensor muscles, from the insertion to the origin, by stretching it 15% to 25%
of its original length (4).
Each tail of the first strip was
applied with the patient’s neck bending and rotating to the opposite site from
the dorsal (T1-T2) to the upper cervical region (C1-C2). The overlying tape,
spaced-strip with openings, was placed perpendicular to the Y-strip, over the
midcervical region (C3-C6), with the patient’s cervical spine in flexion to
apply tension to the posterior structures (5,6).
Patients wore the KT for a 4-week
duration (renewed once a week periodically in this time).
 |
Fig. 1: KT Application
|
Evaluations
- Numeric Rating Scale (NPS-11)
was used to measure pain intensity. The NPS-11 ranges between 0 and 10
(0: minimum pain, 10: maximum pain). It has been shown to be a reliable and
valid tool for the assessment of pain (7).
- The ROM was measured by
using the universal goniometer (8). Neck Disability Index (NDI) was used to
detect functional disability. The NDI consists of 10 questions, and total score
is between 0 and 50 (9).
- For quality of life, the
Short Form-36 Quality of Life Scale (SF-36 QOLS) was used. SF-36 QOLS consists
of 8 subscores: physical function, physical role difficulties (PRD), body pain,
general perception of health, vitality/energy, social function, mental status
role, and mental health. The subscores were calculated separately between 0 and
100 (0: the worst, 100: the best health status). The scores of the 2 main
components (physical score and mental score) were also evaluated. The Turkish
validation was performed by Kocyiğit
et al (10).
- Depressive symptoms were
assessed by the Turkish version of the Beck Depression Inventory (BDI). The
total score was between 0 and 63. Higher total scores indicate more severe
depressive symptoms (11,12).

Discussion
This study revealed that KT is effective treatments for pain, quality of life, and depression in
patients with MNP. We also found that KT may positively influence pain,
disability, and ROM similar to the findings of others (5,6).
It may be possible that the application of KT
provides a proper sensory feedback to the patients, decreasing fear of movement
and thus improving ROM. Because the traction in KT lifts the epidermis
relieving the pressure on the mechanoreceptors below the dermis, therefore
decreasing nociceptive stimuli. Tension in the tape also provides afferent
stimuli facilitating pain inhibition mechanisms, thereby contributing to
reducing pain levels (5).
Conclusions
This study showed that both KT had
a positive impact on pain, disability, quality of life, mood and ROM.

References
1. Fejer
R, Ohm-Kyvik K, Hartvigsen J. The prevalence of neck pain in the world population:
A systematic critical review of the literature. Eur Spine J 2006; 15:834-848.
2. Munoz-Munoz S, Munoz-Garcia MT, Alburquerque-Sendin F,
Arroyo-Morales M, Fernandez-de-las-Penas CJ. Myofascial trigger points, pain, disability and sleep
quality in individuals with mechanical neck pain. Manipulative Physiol Ther
2012; 35:608-613.
3.
Castaldo M, Ge HY, Chiarotto A, Villafane JH, Arendt-Nielsen L. Myofascial trigger
points in patients with whiplashassociated disorders and mechanical neck pain. Pain
Med 2014; 15:842-849.
4.
Saavedra-Hernández M, Castro-Sánchez AM, Cuesta-Vargas AI, Cleland JA, Fernández-de-las-Peñas
C, Arroyo-Morales M. The contribution of previous episodes of pain, pain
intensity, physical impairment, and pain-related fear to disability in patients
with chronic mechanicalneck pain. Am J Phys Med Rehabil 2012;
91:1070-1076.
5.
González-Iglesias J, Fernández-de-Las- Peñas C, Cleland JA, Huijbregts P, Del Rosario
Gutiérrez-Vega M. Short-term effects of cervical kinesio taping on pain and
cervical range of motion in patients with acute whiplash injury: A randomized clinical
trial. J Orthop Sports Phys Ther 2009; 39:515-521.
6.
Saavedra-Hernández M, Castro-Sánchez AM, Arroyo-Morales M, Cleland JA, Lara- Palomo
IC, Fernández-de-Las-Peñas C. Short term effects of kinesio taping versus
cervical thrust manipulation in patients with mechanical neck pain: A randomized
clinical trial. J Orthop Sports Phys Ther 2012; 42:724-730.
7.
Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and
validity of chronic pain intensity measures. Pain 1999; 83:157-162.
8.
Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine
ac tive range of motion in persons with and without neck pain. J Orthop Sports
Phys Ther 2008; 38:640-645.
9.
Macdemid JC, Walton DM, Avery S, et al. Measurement properties of the neck
disability index: A systematic review. J Orthop Sports Phys Ther 2009; 39:400-417.
10.
Koçyiğit H, Aydemir Ö, Fişek G, Ölmez N, Memiş A. The reliability and validity of
Turkish version of Short form 36 (SF 36). J Drug Treat 1995; 12:102-106.
11. Beck
AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression.
Arch Gen Psychiatry 1961; 4:561-571.
12.
Hisli N. Beck Depresyon Envanterinin geçerliği üzerine bir çalışma. Psikoloji
Dergisi 1988; 6:118-122.
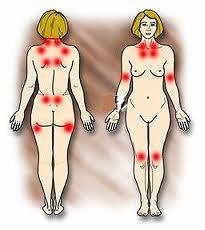
Fibromyalgia
(FM) is a chronic disease characterized by generalized skeletal muscle
pain (1, 2), and other common symptoms include fatigue, sleep disorders,
depression, and excessive anxiety (3–6). The pathogenesis of FM is still not
well understood (7), and FM is considered by some researchers to be a
neurobiological disease caused by abnormal processing of pain (8).
There is currently no cure for FM, but
palliative treatments are available. One type of treatment is strength training (ST). The aim of this
study was to analyze the effects of ST in the treatment of FM through a systematic
review of experimental research. Twenty-two studies were included in
the review. Women aged 18–65 years comprised the total sample and the main
variables analyzed were pain, strength, muscular activity, functional capacity,
fatigue, quality of life, and sleep.
Information extracted from: (Andrade,
A., de Azevedo Klumb Steffens, R., Sieczkowska, S. M., Peyré Tartaruga, L. A.,
& Torres Vilarino, G. (2018). A systematic review of the effects of
strength training in patients with fibromyalgia: clinical outcomes and design
considerations. Advances in Rheumatology, 58(1). doi:10.1186/s42358-018-0033-9).
Results
The analysis of the results revealed
that ST reduced the symptoms of patients with FM, such as pain, fatigue, number
of tender points, depression, and anxiety, with improved functional capacity
and quality of life (9, 10, 11, 12, 13, 14, 15, 16), despite the different training
protocols used.
Pain
Pain was the most studied variable,
showing a reduction after ST (11, 12, 17, 18, 19–21). No study reported
increased pain after or during the intervention period
Muscle
Strength
With regard to muscle strength,
increases between 33 and 63% were observed after 21 and 16 weeks (15, 22).
Quality of
life and Functionality
Studies analysing quality of life and
functionality showed that ST is effective in improving these variables (23, 12,
24, 15, 16, 18).
Depression
The most investigated psychological
variable was depression. The studies of Jones et al. (18), Gavi et al. (12), and
Assumpção et al. (25) showed that ST reduces depressive symptoms; however, the
study of Ericsson et al. (10) did not find a significant difference after 15
weeks of intervention.
Sleep
Quality
We also analyzed the results related
to sleep quality. Andrade et al. (9) found that sleep disorders were reduced after
ST and that sleep correlated with pain. The results of Ericsson et al. (10)
also disclosed that ST yielded better results than relaxation sessions in
improving sleep quality. In addition, another important result is that patients
with FM presented similar responses to those of healthy persons; thus, they
recommended ST to assist in the treatment of patients.
Training Protocol
It was observed that
there is no specific training protocol for patients with FM; thus, the
researchers developed their own protocol.
Intervention protocols
should start at low intensity (40% of 1RM) and gradually increase the
intensity. ST should be performed 2 or 3 times a week to exercise the main
muscle groups. The current studies showed
that ST is a safe and effective method of improving the major symptoms of FM
and can be used to treat patients with this condition.
Example of Training Protocol, Rooks et al. (18)
The intervention was designed to
gradually increase the volume and intensity of exercise a person performed, to
involve all major muscle groups of the body, and to include all 3 aspects of
fitness— cardiovascular endurance, muscle strength, and joint flexibility.
The exercises began with a low volume
of exercise performed at a low intensity, because of the expected lower levels
of cardiovascular fitness and muscle strength reported in women with Fibromyalgia,
and the lower threshold for postexercise muscle pain and fatigue seen in this
population. Participants exercised for 60 minutes per session, 3 times per week
for 20 weeks. The intervention was composed of 2 phases of exercise.
The first
phase (4 weeks) was performed in a pool, and focused on active range of
motion of the body’s major joints. Movements were controlled single-joint
motions.
The second
phase (16 weeks) involved land-based exercises for improving
cardiovascular endurance, muscle strength, and joint range of motion. Each
exercise session was divided into 3 sections—cardiovascular, strength training,
and flexibility—and was always performed in the same order.
- Cardiovascular exercises
incorporated walking on a treadmill (Life Fitness), an elliptical device
(Precor, Bothell, WA), and walking on a track.
- Strength training exercises included
static contractions for pelvic and lumbar spine stabilization, and dynamic
movement of large muscles and multijoint actions: hip flexion/extension, knee
extension/flexion, ankle plantar/dorsiflexion, shoulder flexion, extension,
abduction and horizontal adduction and abduction, elbow flexion and extension,
and trunk flexion and rotation.
Strength training exercises were
performed using a combination of machines (Life Fitness), hand weights, and
body weight. Subjects began with resistance levels they could do easily, and
progressed in an 8-10-12-12 repetition format when appropriate.
- Flexibility was developed using a
complete range of motion during strength training movements, traditional
stretches, and a flexibility device (Precor).
The land-based exercise program was
revised after 3 months to prevent boredom and reduce the chance of dropout.
Conclusion
In conclusion, ST had
positive effects on physical and psychological symptoms, in terms of reducing
pain, the number of tender points, and depression, and improving muscle
strength, sleep quality, functional capacity, and quality of life.
Bibliography
1. Wolfe F, Smythe HA,
Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College
of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis
Rheum. 1990;33(2):160–72.
2. Wolfe F, Clauw DJ,
Fitzcharles M-A, Goldenberg DL, Häuser W, Katz RL, et al. 2016 Revisions to the
2010/2011 fibromyalgia diagnostic criteria. Seminars in arthritis and
rheumatism. 2016;46:319-29.
3. Wolfe F, Clauw DJ,
Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. The American College of
Rheumatology Preliminary Diagnostic Criteria for fibromyalgia and measurement
of symptom severity. Arthritis Care Res. 2010;62(5):600–10 PubMed PMID:
WOS:000280979600004.
4. Borchers AT, Gershwin
ME. Fibromyalgia: a critical and comprehensive review. Clin Rev Allergy
Immunol. 2015;49(2):100–51 PubMed PMID:WOS: 000362902500002.English.
5. McDowell CP, Cook DB,
Herring MP. The effects of exercise training on anxiety in fibromyalgia
patients: a meta-analysis. Med Sci Sports Exerc. 2017; 49(9):1868–76 PubMed
PMID: 28419024.Epub 2017/04/19.eng.
6. Häuser W, Ablin J,
Fitzcharles M-A, Littlejohn G, Luciano JV, Usui C, et al. Fibromyalgia. Nature
reviews Disease primers. 2015;1:15022.
7. Andrade A, Vilarino
GT, Sieczkowska SM, Coimbra DR, Steffens RAK, Vietta GG. Acute effects of
physical exercises on the inflammatory markers of patients with fibromyalgia
syndrome: a systematic review. J Neuroimmunol. 2018;316:40–9.
8. Sluka KA, Clauw DJ.
Neurobiology of fibromyalgia and chronic widespread pain.
9. Andrade A, Vilarino GT,
Bevilacqua GG. What is the effect of strength training on pain and sleep in
patients with fibromyalgia? Am J Phys Med Rehabil. 2017.
10. Ericsson A, Palstam
A, Larsson A, Lofgren M, Bileviciute-Ljungar I, Bjersing J, et al. Resistance
exercise improves physical fatigue in women with fibromyalgia: a randomized
controlled trial. Arthritis Res Ther. 2016;18:12 PubMed PMID:
WOS:000381728500002. English.
11. Kingsley JD,
McMillan V, Figueroa A. The effects of 12 weeks of resistance exercise training
on disease severity and autonomic modulation at rest and after acute leg
resistance exercise in women with fibromyalgia. Arch Phys Med Rehabil.
2010;91(10):1551–7 PubMed PMID: WOS:000282720300010. English.
12. Gavi M, Vassalo DV, Amaral FT, DCF M, Gava PL, Dantas
EM, et al. Strengthening exercises improve symptoms and quality
of life but do not change autonomic modulation in fibromyalgia: a randomized
clinical trial. PLoS One. 2014;9(3):–8 PubMed PMID: WOS:000333352800023.
English.
13. Hakkinen A, Hakkinen
K, Hannonen P, Alen M. Strength training induced adaptations in neuromuscular
function of premenopausal women with fibromyalgia: comparison with healthy
women. Ann Rheum Dis. 2001;60(1): 21–6 PubMed PMID: WOS:000166008100005.
English.
14. Martinsen S, Flodin
P, Berrebi J, Lofgren M, Bileviciute-Ljungar I, Mannerkorpi K, et al. The role
of long-term physical exercise on performance and brain activation during the
Stroop colour word task in fibromyalgia patients. Clin Physiol Funct Imaging.
2017; PubMed PMID: 28627125. Epub 2017/06/20. eng.
15. Valkeinen H, Alen M,
Hannonen P, Hakkinen A, Airaksinen O, Hakkinen K. Changes in knee extension and
flexion force, EMG and functional capacity during strength training in older females
with fibromyalgia and healthy controls. Rheumatology. 2004;43(2):225–8 PubMed
PMID: WOS:000188850000018.
English.
16. Bircan C, Karasel
SA, Akgun B, El O, Alper S. Effects of muscle strengthening versus aerobic
exercise program in fibromyalgia. Rheumatol Int. 2008;28(6): 527–32 PubMed
PMID: WOS:000254206100004. English.
17. Hooten WM, Qu WC,
Townsend CO, Judd JW. Effects of strength vs aerobic exercise on pain severity
in adults with fibromyalgia: A randomized equivalence trial. Pain.
2012;153(4):915–923. PubMed PMID: WOS: 000301877300027. English.
18. Rooks DS, Silverman
CB, Kantrowitz FG. The effects of progressive strength training and aerobic
exercise on muscle strength and cardiovascular fitness in women with
fibromyalgia: a pilot study. Arthritis Rheum-Arthritis Care Res.
2002;47(1):22–8 PubMed PMID: WOS:000173803700005. English.
19. Valkeinen H,
Hakkinen A, Hannonen P, Hakkinen K, Alen M. Acute heavyresistance exercise-induced
pain and neuromuscular fatigue in elderly women with fibromyalgia and in
healthy controls - effects of strength training. Arthritis Rheum.
2006;54(4):1334–9 PubMed PMID: WOS:000236830800035.
English.
20. Larsson A, Palstam
A, Lofgren M, Ernberg M, Bjersing J, Bileviciute-Ljungar I, et al. Resistance
exercise improves muscle strength, health status and pain intensity in
fibromyalgia-a randomized controlled trial. Arthritis Research & Therapy.
2015;17:15 PubMed PMID: WOS:000357248900001. English.
21. Palstam A, Larsson
A, Lofgren M, Ernberg M, Bjersing J, Bileviciute-Ljungar I, et al. Decrease of
fear avoidance beliefs following person-centered progressive resistance
exercise contributes to reduced pain disability in women with fibromyalgia:
secondary exploratory analyses from a randomized controlled trial. Arthritis
Research & Therapy. 2016;18 PubMed PMID: WOS:000376372300006.
22. Figueroa A, Kingsley JD, McMillan V, Panton LB. Resistance
exercise training improves heart rate variability in women with fibromyalgia.
Clin Physiol Funct Imaging. 2008;28(1):49–54 PubMed PMID: WOS:000251629100008.
23. Kingsley JD, Panton
LB, Toole T, Sirithienthad P, Mathis R, McMillan V. The effects of a 12-week
strength-training program on strength and functionality in women with
fibromyalgia. Arch Phys Med Rehabil. 2005; 86(9):1713–21 PubMed PMID:
WOS:000231747300001.
24. Panton LB, Figueroa
A, Kingsley JD, Hornbuckle L, Wilson J, St John N, et al. Effects of resistance
training and chiropractic treatment in women with fibromyalgia. J Altern
Complement Med. 2009;15(3):321–8 PubMed PMID: 19249999. Epub 2009/03/03. eng.
25. Assumpção A ML, Yuan
SL, Santos AS, Sauer J, Mango P, Marques AP. Muscle stretching exercises and
resistance training in fibromyalgia: which is better? A three-arm randomized
controlled trial. - PubMed - NCBI. 2017.