In recent years, running has increased its popularity in our
society, breaking records of participation in various popular races. In each of
our cities we can observe a large number of “runners” alone or in groups trying
to improve their brands or simply enjoying the sport.
Most runners have suffered an injury throughout their lives,
covering problems from the foot to the cervical level. In this article we will
analyze the most common injuries in runners and how to prevent or treat them.
The body gives us warning signs, the following phrases will
sound: "Uff, how loaded I am", "today it was difficult for me to
get in bed", "I have noticed a pull on the leg"
Physiotherapy can help us not to say these phrases or, if it
is too late, to prevent further injury. Listen to your body and consult your
physiotherapist with any questions and do not hesitate to call us for any
questions.
The most common injuries are: plantar fasciitis, iliotibial
girdle, tibial periostitis, tedinopathies, sprains and muscle tears.
- Plantar fasciitis: the plantar fascia is defined as a
fibrous and elastic tissue, which covers most of the sole of the foot, and that
originates in the calcaneus bone (heel bone), until it is inserted into the
base of the metatarsals (fingers) It is responsible for stabilizing and
supporting the entire foot assembly; joints and plantar arch.
There are several causes or risk
factors for which it can occur are: the increase in physical or sports load, or
sudden change in it; plantar arch alteration, whether increased or decreased
(cavus or flatfoot); tension or retraction of the Achilles tendon;
inappropriate footwear; Obesity or sudden weight gain.
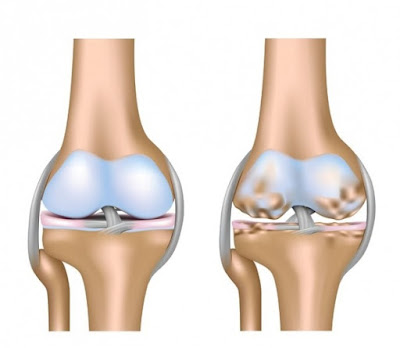
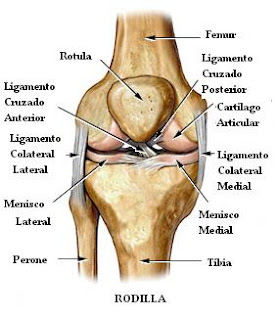
- Iliotibial waist: it is an inflammation that occurs in the
lateral or external area of the knee, caused by the friction caused between
the lateral condyle of the femur and the iliotibial waistband. It is usually a
very typical pain in runners, due to bad biomechanics of the race when the
muscles are fatigued. The main problem is the failure of the gluteus medius in monopodial
support causing the knee to go further in each step and the friction described
above occurs.
- Shin Splints: pain located along the two distal
thirds of the posterior medial tibia during exercise, with pain in the
palpation of the tibia. It is caused by overloading of the tibial bone cortex,
resulting in an inflammation of the membrane that covers the bone.
The risk factors
by which it can occur are: increase in body mass; non-progressive increase in
training; flat foot, a bad biomechanics of tread produces adaptations of other
areas of the body and can affect the tibia; lack of range of motion in the
ankle; lack of range of movement in the hip: the lack of strength in the
gluteus medius triggers a valgus knee and, as a consequence, an incorrect tread;
run on hard surfaces.
- Tendinopathies: Tendonitis is a very frequent pathology,
which usually appears after excessive efforts, repetitive movements and direct
trauma. It consists of the inflammation of the tendons, which are resistant
strings of tissue that link the muscles with the bones and help the muscles
move the bones.
Avoid repetitive movements and overload, keep the muscles
strong and flexible, exercise the upper and lower extremities, without
excessively repeating the same movement, alternating different types of
movements, with small recovery intervals. Good hydration is also recommended,
as it always helps to maintain a better vascularization of the area.
- Sprains: it is an elongation or rupture of the ligaments
that slow the inversion of the foot. We must perform balance or proprioception
exercises to improve the position of the ankle at the nervous system level and
strengthen the muscles that are responsible for maintaining a correct
positioning of the foot.
- Muscle tears: it is the separation or lack of congruence
of muscle fibers. Whether you are a sports person or if you are more sedentary,
a key aspect is to keep the body hydrated. If any sporting activity is carried
out, it is essential to perform a good warm-up prior to it, because that way we
can prepare the muscles for the activity, so that they can react quickly and
correctly.
In addition, resting times are essential. If we do not rest
properly between workouts we will have fatigued muscles, so that they will be
unable to adapt effectively to the activity to which we are subjected. It is
very important to let the muscle recover. In the case of runners, muscle
overload can lead to muscle breakage due to changes in pace or high running
intensities. That is why it is very important to treat the affected muscles to
prevent it from going further. The body is warning us and we must listen.