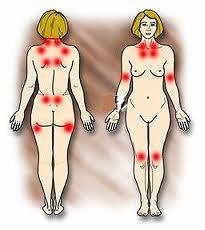
Fibromyalgia
(FM) is a chronic disease characterized by generalized skeletal muscle
pain (1, 2), and other common symptoms include fatigue, sleep disorders,
depression, and excessive anxiety (3–6). The pathogenesis of FM is still not
well understood (7), and FM is considered by some researchers to be a
neurobiological disease caused by abnormal processing of pain (8).
There is currently no cure for FM, but
palliative treatments are available. One type of treatment is strength training (ST). The aim of this
study was to analyze the effects of ST in the treatment of FM through a systematic
review of experimental research. Twenty-two studies were included in
the review. Women aged 18–65 years comprised the total sample and the main
variables analyzed were pain, strength, muscular activity, functional capacity,
fatigue, quality of life, and sleep.
Information extracted from: (Andrade,
A., de Azevedo Klumb Steffens, R., Sieczkowska, S. M., Peyré Tartaruga, L. A.,
& Torres Vilarino, G. (2018). A systematic review of the effects of
strength training in patients with fibromyalgia: clinical outcomes and design
considerations. Advances in Rheumatology, 58(1). doi:10.1186/s42358-018-0033-9).
Results
The analysis of the results revealed
that ST reduced the symptoms of patients with FM, such as pain, fatigue, number
of tender points, depression, and anxiety, with improved functional capacity
and quality of life (9, 10, 11, 12, 13, 14, 15, 16), despite the different training
protocols used.
Pain
Pain was the most studied variable,
showing a reduction after ST (11, 12, 17, 18, 19–21). No study reported
increased pain after or during the intervention period
Muscle
Strength
With regard to muscle strength,
increases between 33 and 63% were observed after 21 and 16 weeks (15, 22).
Quality of
life and Functionality
Studies analysing quality of life and
functionality showed that ST is effective in improving these variables (23, 12,
24, 15, 16, 18).
Depression
The most investigated psychological
variable was depression. The studies of Jones et al. (18), Gavi et al. (12), and
Assumpção et al. (25) showed that ST reduces depressive symptoms; however, the
study of Ericsson et al. (10) did not find a significant difference after 15
weeks of intervention.
Sleep
Quality
We also analyzed the results related
to sleep quality. Andrade et al. (9) found that sleep disorders were reduced after
ST and that sleep correlated with pain. The results of Ericsson et al. (10)
also disclosed that ST yielded better results than relaxation sessions in
improving sleep quality. In addition, another important result is that patients
with FM presented similar responses to those of healthy persons; thus, they
recommended ST to assist in the treatment of patients.
Training Protocol
It was observed that
there is no specific training protocol for patients with FM; thus, the
researchers developed their own protocol.
Intervention protocols
should start at low intensity (40% of 1RM) and gradually increase the
intensity. ST should be performed 2 or 3 times a week to exercise the main
muscle groups. The current studies showed
that ST is a safe and effective method of improving the major symptoms of FM
and can be used to treat patients with this condition.
Example of Training Protocol, Rooks et al. (18)
The intervention was designed to
gradually increase the volume and intensity of exercise a person performed, to
involve all major muscle groups of the body, and to include all 3 aspects of
fitness— cardiovascular endurance, muscle strength, and joint flexibility.
The exercises began with a low volume
of exercise performed at a low intensity, because of the expected lower levels
of cardiovascular fitness and muscle strength reported in women with Fibromyalgia,
and the lower threshold for postexercise muscle pain and fatigue seen in this
population. Participants exercised for 60 minutes per session, 3 times per week
for 20 weeks. The intervention was composed of 2 phases of exercise.
The first
phase (4 weeks) was performed in a pool, and focused on active range of
motion of the body’s major joints. Movements were controlled single-joint
motions.
The second
phase (16 weeks) involved land-based exercises for improving
cardiovascular endurance, muscle strength, and joint range of motion. Each
exercise session was divided into 3 sections—cardiovascular, strength training,
and flexibility—and was always performed in the same order.
- Cardiovascular exercises
incorporated walking on a treadmill (Life Fitness), an elliptical device
(Precor, Bothell, WA), and walking on a track.
- Strength training exercises included
static contractions for pelvic and lumbar spine stabilization, and dynamic
movement of large muscles and multijoint actions: hip flexion/extension, knee
extension/flexion, ankle plantar/dorsiflexion, shoulder flexion, extension,
abduction and horizontal adduction and abduction, elbow flexion and extension,
and trunk flexion and rotation.
Strength training exercises were
performed using a combination of machines (Life Fitness), hand weights, and
body weight. Subjects began with resistance levels they could do easily, and
progressed in an 8-10-12-12 repetition format when appropriate.
- Flexibility was developed using a
complete range of motion during strength training movements, traditional
stretches, and a flexibility device (Precor).
The land-based exercise program was
revised after 3 months to prevent boredom and reduce the chance of dropout.
Conclusion
In conclusion, ST had
positive effects on physical and psychological symptoms, in terms of reducing
pain, the number of tender points, and depression, and improving muscle
strength, sleep quality, functional capacity, and quality of life.
Bibliography
1. Wolfe F, Smythe HA,
Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College
of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis
Rheum. 1990;33(2):160–72.
2. Wolfe F, Clauw DJ,
Fitzcharles M-A, Goldenberg DL, Häuser W, Katz RL, et al. 2016 Revisions to the
2010/2011 fibromyalgia diagnostic criteria. Seminars in arthritis and
rheumatism. 2016;46:319-29.
3. Wolfe F, Clauw DJ,
Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. The American College of
Rheumatology Preliminary Diagnostic Criteria for fibromyalgia and measurement
of symptom severity. Arthritis Care Res. 2010;62(5):600–10 PubMed PMID:
WOS:000280979600004.
4. Borchers AT, Gershwin
ME. Fibromyalgia: a critical and comprehensive review. Clin Rev Allergy
Immunol. 2015;49(2):100–51 PubMed PMID:WOS: 000362902500002.English.
5. McDowell CP, Cook DB,
Herring MP. The effects of exercise training on anxiety in fibromyalgia
patients: a meta-analysis. Med Sci Sports Exerc. 2017; 49(9):1868–76 PubMed
PMID: 28419024.Epub 2017/04/19.eng.
6. Häuser W, Ablin J,
Fitzcharles M-A, Littlejohn G, Luciano JV, Usui C, et al. Fibromyalgia. Nature
reviews Disease primers. 2015;1:15022.
7. Andrade A, Vilarino
GT, Sieczkowska SM, Coimbra DR, Steffens RAK, Vietta GG. Acute effects of
physical exercises on the inflammatory markers of patients with fibromyalgia
syndrome: a systematic review. J Neuroimmunol. 2018;316:40–9.
8. Sluka KA, Clauw DJ.
Neurobiology of fibromyalgia and chronic widespread pain.
9. Andrade A, Vilarino GT,
Bevilacqua GG. What is the effect of strength training on pain and sleep in
patients with fibromyalgia? Am J Phys Med Rehabil. 2017.
10. Ericsson A, Palstam
A, Larsson A, Lofgren M, Bileviciute-Ljungar I, Bjersing J, et al. Resistance
exercise improves physical fatigue in women with fibromyalgia: a randomized
controlled trial. Arthritis Res Ther. 2016;18:12 PubMed PMID:
WOS:000381728500002. English.
11. Kingsley JD,
McMillan V, Figueroa A. The effects of 12 weeks of resistance exercise training
on disease severity and autonomic modulation at rest and after acute leg
resistance exercise in women with fibromyalgia. Arch Phys Med Rehabil.
2010;91(10):1551–7 PubMed PMID: WOS:000282720300010. English.
12. Gavi M, Vassalo DV, Amaral FT, DCF M, Gava PL, Dantas
EM, et al. Strengthening exercises improve symptoms and quality
of life but do not change autonomic modulation in fibromyalgia: a randomized
clinical trial. PLoS One. 2014;9(3):–8 PubMed PMID: WOS:000333352800023.
English.
13. Hakkinen A, Hakkinen
K, Hannonen P, Alen M. Strength training induced adaptations in neuromuscular
function of premenopausal women with fibromyalgia: comparison with healthy
women. Ann Rheum Dis. 2001;60(1): 21–6 PubMed PMID: WOS:000166008100005.
English.
14. Martinsen S, Flodin
P, Berrebi J, Lofgren M, Bileviciute-Ljungar I, Mannerkorpi K, et al. The role
of long-term physical exercise on performance and brain activation during the
Stroop colour word task in fibromyalgia patients. Clin Physiol Funct Imaging.
2017; PubMed PMID: 28627125. Epub 2017/06/20. eng.
15. Valkeinen H, Alen M,
Hannonen P, Hakkinen A, Airaksinen O, Hakkinen K. Changes in knee extension and
flexion force, EMG and functional capacity during strength training in older females
with fibromyalgia and healthy controls. Rheumatology. 2004;43(2):225–8 PubMed
PMID: WOS:000188850000018.
English.
16. Bircan C, Karasel
SA, Akgun B, El O, Alper S. Effects of muscle strengthening versus aerobic
exercise program in fibromyalgia. Rheumatol Int. 2008;28(6): 527–32 PubMed
PMID: WOS:000254206100004. English.
17. Hooten WM, Qu WC,
Townsend CO, Judd JW. Effects of strength vs aerobic exercise on pain severity
in adults with fibromyalgia: A randomized equivalence trial. Pain.
2012;153(4):915–923. PubMed PMID: WOS: 000301877300027. English.
18. Rooks DS, Silverman
CB, Kantrowitz FG. The effects of progressive strength training and aerobic
exercise on muscle strength and cardiovascular fitness in women with
fibromyalgia: a pilot study. Arthritis Rheum-Arthritis Care Res.
2002;47(1):22–8 PubMed PMID: WOS:000173803700005. English.
19. Valkeinen H,
Hakkinen A, Hannonen P, Hakkinen K, Alen M. Acute heavyresistance exercise-induced
pain and neuromuscular fatigue in elderly women with fibromyalgia and in
healthy controls - effects of strength training. Arthritis Rheum.
2006;54(4):1334–9 PubMed PMID: WOS:000236830800035.
English.
20. Larsson A, Palstam
A, Lofgren M, Ernberg M, Bjersing J, Bileviciute-Ljungar I, et al. Resistance
exercise improves muscle strength, health status and pain intensity in
fibromyalgia-a randomized controlled trial. Arthritis Research & Therapy.
2015;17:15 PubMed PMID: WOS:000357248900001. English.
21. Palstam A, Larsson
A, Lofgren M, Ernberg M, Bjersing J, Bileviciute-Ljungar I, et al. Decrease of
fear avoidance beliefs following person-centered progressive resistance
exercise contributes to reduced pain disability in women with fibromyalgia:
secondary exploratory analyses from a randomized controlled trial. Arthritis
Research & Therapy. 2016;18 PubMed PMID: WOS:000376372300006.
22. Figueroa A, Kingsley JD, McMillan V, Panton LB. Resistance
exercise training improves heart rate variability in women with fibromyalgia.
Clin Physiol Funct Imaging. 2008;28(1):49–54 PubMed PMID: WOS:000251629100008.
23. Kingsley JD, Panton
LB, Toole T, Sirithienthad P, Mathis R, McMillan V. The effects of a 12-week
strength-training program on strength and functionality in women with
fibromyalgia. Arch Phys Med Rehabil. 2005; 86(9):1713–21 PubMed PMID:
WOS:000231747300001.
24. Panton LB, Figueroa
A, Kingsley JD, Hornbuckle L, Wilson J, St John N, et al. Effects of resistance
training and chiropractic treatment in women with fibromyalgia. J Altern
Complement Med. 2009;15(3):321–8 PubMed PMID: 19249999. Epub 2009/03/03. eng.
25. Assumpção A ML, Yuan
SL, Santos AS, Sauer J, Mango P, Marques AP. Muscle stretching exercises and
resistance training in fibromyalgia: which is better? A three-arm randomized
controlled trial. - PubMed - NCBI. 2017.
Knee osteoarthritis (OA) is the most prevalent chronic joint
disease. Cartilage is the central tissue affected by OA and causes subsequent
symptoms, including joint pain, stiffness and joint swelling, which diminishes
the range of motion (1,2).
Currently, no reliable treatment has been confirmed to
prevent progression of knee OA. The aim this review was to evaluate the
efficacy of Kinesio Taping (KT) in reducing pain and increasing knee function in
patients with OA.
 |
| Knee osteoarthritis |
(Information extracted from: Lu, Zhijun, et al. "Kinesio
taping improves pain and function in patients with knee osteoarthritis: A
meta-analysis of randomized controlled trials." International Journal of
Surgery (2018))
Kinesio Taping Application
Five studies were included in this review. They compared an
intervention group who received KT to a placebo group received
sham Taping.
1. Cho et
al. (3) an I-shaped KT starting at the origin of the rectus femoris and a Y-shaped
KT proximal to the superior patellar boarder. While KT was applied, the
quadriceps muscle was being stretched.
 |
| Cho et al. |
2. Wageck et
al. (4) three KT elements applied simultaneously.
A) Drainage element of the
experimental application. B) Muscle strength element of the experimental
application. C) Pain-relief
element of the experimental application. D) Combined experimental application.
 |
| Wageck et al. |
3. Mutlu et
al. (5) KT on their quadriceps femoris and hamstring muscle. First,
patients were taped with a Y-shaped Kinesio type at the quadriceps femoris. The
tape was applied a point 5 cm inferior to the anterior superior iliac spine to
the knee cap (origin to insertion), with the patient in a supine position with
25% tension. Then, each patient flexed his or her knee, and the Y-shaped tape
(the tails of the tape) was circled around the patella, ending at its inferior
side with no tension.
Next, patients were
taped with a Y-shaped Kinesio type at the hamstring muscle. The tape was
applied from ischial tuberosity to the back of the knee, with the patients in a
standing position with their trunk bent. Then, the Y-shaped tape (the tails of
the tape) was applied around the lateral side of the knee and medial side of
the knee.
 |
| Mutlu et al. |
4. Aydogdu
et al. (6) KT on quadriceps and hamstring muscles was performed with Y-shaped
technique. The subjects lay in the supine position with the hip flexed
at 30◦ and the knee flexed at 60◦. In the supine position, taping was first
applied to the quadriceps femoris. The tape was applied from a point 10 cm
inferior to the anterior superior iliac spine, bisected at the junction between
quadriceps femoris tendon and the patella, and circled around the patella,
ending at its inferior side. The first 5 cm of the tape were not stretched. The
portion between the first part of tape and superior patella was stretched to
50–70%. The remaining tape around the patella remained un-stretched. After
that, in the prone position, hamstring was taped secondly with the same method.
 |
| Aydogdu et al. |
5. Rahlf et
al. (7) KT on their quadriceps femoris and hamstring muscle. A medial
and a lateral “I” strap as well as 1 “I” strap over the patella were applied.
“I” strap means the tape is not cut into different parts; The strap across the
patella was applied in individual maximum knee flexion. The base of the tape
was applied at the tibial tuberosity and pulled in maximum tension over the
patella, ending at the lower third of the quadriceps femoris muscle. The medial
and lateral straps were applied in 45° knee flexion along the collateral medial
and lateral ligaments.
 |
| Rahlf et al. |
Outcomes after place
KT
Visual analog scale (VAS)
VAS scale was adopted to measure pain and it was considered
a subjective method.
Taping was associated with a significantly reduction in VAS
scale at rest, as well as at movement in patients with knee OA. This pain
reduction can be attributed to neurological suppression, due to stimulation of
cutaneous mechanoreceptors.
Anandkumar et al. (8) showed that there was a decreased pain
in Kinesio Taping groups while climbing stairs. The present meta-analysis
indicated that Kinesio Taping was associated with a significantly reduction in
VAS scale at rest.
Range of motion and McMaster Universities Arthritis Index
(WOMAC) scale
Articular cartilage can be damaged by normal wear and
abnormal mechanical loading which may cause abnormal cellular activities in
cartilage and synovium, resulting in stiffness, loss of range of motion (9).
Our review demonstrated that Kinesio Taping was associated
with an improved WOMAC compared with sham Taping. So Kinesio Taping could
significantly improve knee flexion range of motion.
Muscle strength
Quadriceps
femoris muscle weakness is a common symptom in knee OA and this may affect
joint function and accelerate progress of degeneration (10,11). There was no significant difference in quadriceps femoris
muscle in patients with knee OA.
Conclusions
Kinesio Taping is effective in improving for pain and joint function
in patients with knee OA.
Bibliography
1. M.
Hurley, K. Dickson, R. Hallett, R. Grant, H. Hauari, N. Walsh, C. Stansfield, S.
Oliver, Exercise interventions and patient beliefs for people with hip, knee or
hip and knee osteoarthritis: a mixed methods review, Cochrane Database Syst.
Rev. 4 (2018) CD010842.
2. S.
Demehri, D. Shakoor, Structural Changes in Aging-knee versus Early-knee Osteoarthritis:
Review of Current Evidence and Future Challenges, Osteoarthritis and cartilage,
2018.
3. H.Y.
Cho, E.H. Kim, J. Kim, Y.W. Yoon, Kinesio taping improves pain, range of motion,
and proprioception in older patients with knee osteoarthritis: a randomized controlled
trial, Am. J. Phys. Med. Rehabil. 94 (3) (2015) 192–200.
4. B.
Wageck, G.S. Nunes, N.B. Bohlen, G.M. Santos, M. de Noronha, Kinesio Taping does
not improve the symptoms or function of older people with knee osteoarthritis: a
randomised trial, J. Physiother. 62 (3) (2016) 153–158.
5. E.
Kaya Mutlu, R. Mustafaoglu, T. Birinci, A. Razak Ozdincler, Does kinesio taping
of the knee improve pain and functionality in patients with knee
osteoarthritis?: a randomized controlled clinical trial, Am. J. Phys. Med.
Rehabil. 96 (1) (2017) 25–33.
6. O.
Aydogdu, Z. Sari, S.U. Yurdalan, M.G. Polat, Clinical outcomes of kinesio
taping applied in patients with knee osteoarthritis: a randomized controlled
trial, J. Back Musculoskelet. Rehabil. 30 (5) (2017) 1045–1051.
7. A.L.
Rahlf, K.M. Braumann, A. Zech, Kinesio taping improves perceptions of pain and
function of patients with knee osteoarthritis. A randomized, controlled trial,
J. Sport Rehabil. (2018) 1–21.
8. S.
Anandkumar, S. Sudarshan, P. Nagpal, Efficacy of kinesio taping on isokinetic quadriceps
torque in knee osteoarthritis: a double blinded randomized controlled study,
Physiother. Pract. 30 (6) (2014) 375–383.
9. D.
Chen, J. Shen, W. Zhao, T. Wang, L. Han, J.L. Hamilton, H.J. Im,
Osteoarthritis: toward a comprehensive understanding of pathological mechanism,
Bone Res. 5 (1) (2017) 1–13.
10. C. Slemenda,
D.K. Heilman, K.D. Brandt, B.P. Katz, S.A. Mazzuca, E.M. Braunstein, D. Byrd,
Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis
in women? Arthritis Rheum. 41 (11) (1998) 1951–1959.
11.
M.B. Conroy, C.K. Kwoh, E. Krishnan, M.C. Nevitt, R. Boudreau, L.D. Carbone, H.
Chen, T.B. Harris, A.B. Newman, B.H. Goodpaster, Muscle strength, mass, and quality
in older men and women with knee osteoarthritis, Arthritis Care Res. 64 (1) (2012)
15–21.